Introduction
The rise of antimicrobial resistance (AMR) poses a serious threat to global health, with the World Health Organization (WHO) identifying it as one of the most pressing health issues of our time. As conventional antibiotics become less effective against resistant strains of bacteria, researchers and healthcare professionals are increasingly turning to alternative treatments to combat infections. One of the most promising alternatives is phage therapy, an innovative approach that harnesses the power of bacteriophages—viruses that specifically infect and kill bacteria. In this article we will explore the mechanisms of phage therapy, its historical context, current applications, regulatory considerations, the role of phage biobanks, pros and cons and future directions.
What is Phage Therapy?
Phage therapy involves using bacteriophages to target and eliminate specific bacterial strains. Unlike antibiotics, which can indiscriminately kill both harmful and beneficial bacteria, phages are highly specific. This specificity minimises collateral damage to the body’s microbiome, making phage therapy an attractive option for treating bacterial infections, especially those resistant to conventional antibiotics.
Historical Background of Phage Therapy
The concept of using phages to treat bacterial infections dates back to the early 20th century. The pioneering work of Félix d’Hérelle in 1917 marked the beginning of phage therapy. D’Hérelle discovered that certain viruses could infect and kill bacteria, and he successfully treated patients with dysentery using phage preparations (Abedon, 2019). However, the introduction of antibiotics in the 1940s overshadowed phage therapy, leading to its decline in Western medicine. Recently, interest in phage therapy has resurfaced due to the alarming rise in antibiotic-resistant infections (Holt, 2017).
How Phages Work
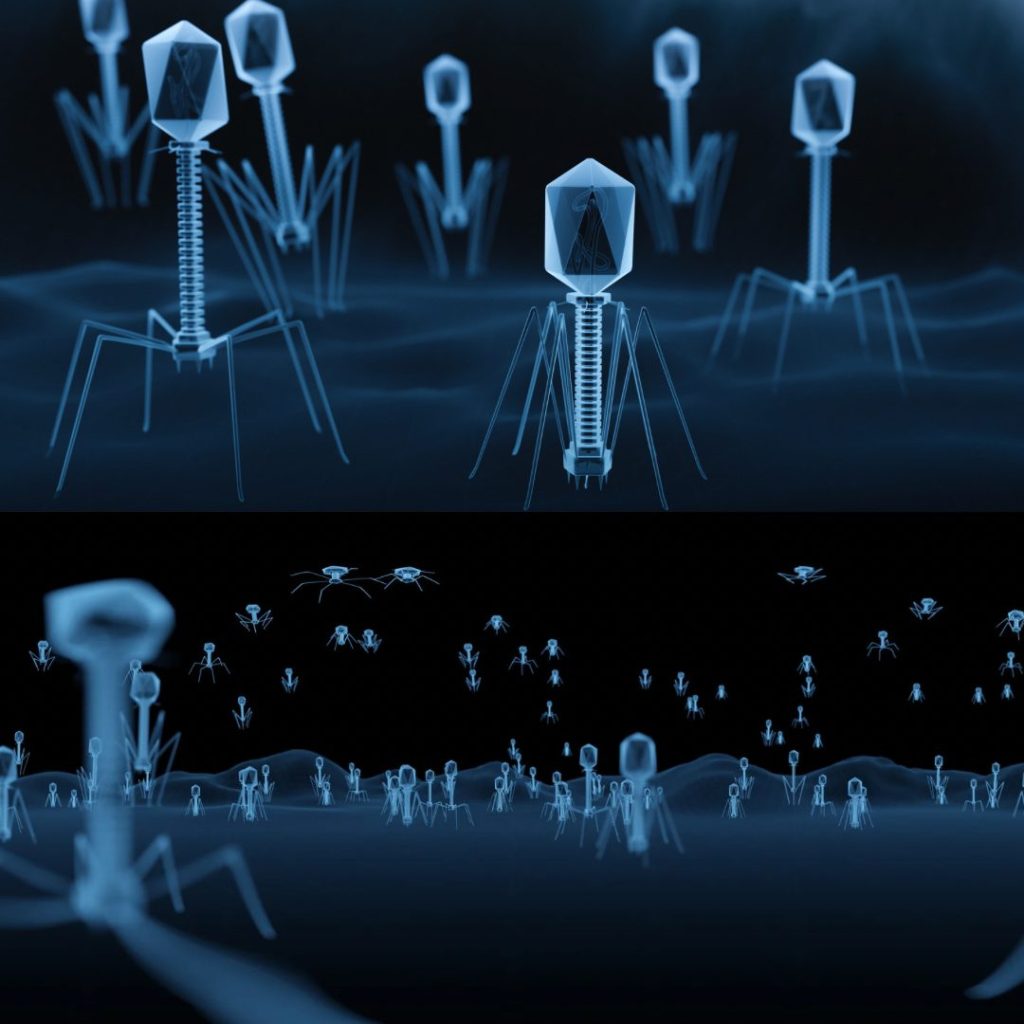
Bacteriophages have a unique lytic lifecycle that allows them to infect and kill bacteria effectively. The process involves several stages:
- Attachment: Phages recognise and bind to specific bacterial cells via receptor molecules on the surface of the bacteria, using their tail fibres to identify suitable targets.
- Injection: Once attached, the phage injects its genetic material into the bacterium.
- Replication: The phage hijacks the bacterium’s cellular machinery to replicate its genetic material and produce new phage components.
- Assembly: The newly produced phage components assemble into fully functional phages.
- Lysis: The bacterial cell ultimately lyses, releasing new phages into the surrounding environment to infect neighbouring bacteria (Hyman & Abedon, 2010).
This specificity and efficiency make phages a powerful tool in combatting bacterial infections, especially those that resist conventional treatments.
Current Applications of Phage Therapy
Phage therapy is gaining traction in various medical fields, particularly in treating infections that are difficult to manage with traditional antibiotics. Here are some key areas where phage therapy is currently being utilised:
- Compassionate Use Cases: Phage therapy has been administered in compassionate use situations, where patients with severe, multidrug-resistant infections have received phage treatments when no other options were available. Documented cases have shown success in treating infections in cystic fibrosis patients and those with chronic wounds.
- Clinical Trials: Several clinical trials are ongoing to evaluate the safety and efficacy of phage therapy for different types of infections, including respiratory infections, chronic wounds, and gastrointestinal conditions. These trials are essential for gathering data to support regulatory approval and broader clinical use.
- Research Institutions: Various research centres and institutions are actively studying phage therapy, exploring its potential applications, and developing phage preparations. For instance, the Felix d’Hérelle Reference Centre for Bacterial Viruses at the University of Leicester plays a significant role in phage research.
- Regulatory Developments: Countries like the UK have established regulatory frameworks to support the development and use of phage therapy. The Medicines and Healthcare products Regulatory Agency (MHRA) has issued guidance to facilitate the safe use of phage therapy products.
- Commercial Products: Some companies are working on developing phage-based products for clinical use, aiming to make phage therapy more widely available as a treatment option.
The Role of Phage Biobanks
Phage biobanks are essential for the advancement of phage therapy, as they provide a systematic collection of bacteriophages that can be used for research and clinical applications. A biobank can be broadly defined as a repository for biological samples, including phages, which are organised and intended for research use (Hewitt & Watson, 2013).
How Is a Phage Biobank Maintained?
Maintaining a phage biobank involves more than simply freezing and storing samples. Each isolated phage undergoes genetic sequencing, testing against a panel of bacterial strains, and regular re-evaluation to ensure its activity remains stable (Lin et al., 2021). Comprehensive records must be kept about the origin, infectivity, and characteristics of each phage, making this information easily accessible for clinicians or researchers.
Clinical Workflow with Phage Biobanks
When a patient presents with a resistant bacterial infection, clinicians can isolate the bacterial strain and screen it against phage libraries to identify the most effective viral candidates (Chan et al., 2013). Selected phages are then combined into cocktails to ensure broad activity and minimise the development of bacterial resistance (Schooley et al., 2017). Phage biobanks are invaluable in this process, as they provide the diverse libraries needed to create personalised phage cocktails tailored to individual infections (Dedrick et al., 2019).
A Citizen-Driven Approach
What distinguishes this approach is that it is citizen-driven. By involving the public in phage collection, there is an aim to enhance the ecological and genetic diversity of the phage biobank, increasing the likelihood of finding matches for even the most stubborn infections. Society has a moral obligation to participate in the fight against the evolving landscape of bacterial infections, as the invisible threat of AMR becomes increasingly visible (Anomaly, 2020).
Philosopher Gerald Gaus’s public harm principle illustrates the importance of collective action in addressing public problems like antibiotic-resistant infections. When a significant issue arises from the actions of many individuals, and no single person can resolve it, collective action is necessary (Gaus, 1998). The phage biobank enables everyone to contribute to a viable solution in combating dangerous infections.
Ethics and Equity
Involving the public in phage collection raises important ethical considerations. Questions arise regarding ownership of life-saving phages found in private spaces and ensuring global access to these therapies, especially given that most biobanks are developed in wealthier countries while the worst cases of drug resistance are often found in poorer regions (Anomaly, 2020). The solution lies not only in better science but also in establishing equitable systems. The lab aims to build an open-source phage biobank that fosters global collaboration.
To transition from scientific theory to patient treatment, phage therapies require rigorous clinical trials, which depend on having well-organised and thoroughly studied collections of phages. With the necessary infrastructure in place, researchers can quickly develop personalised phage treatments and conduct high-quality clinical trials, meeting the requirements of health systems and regulators. Without robust clinical trials to assess the safety and efficacy of phages, their potential will remain limited.
When Will Phage Therapy Be Widely Available?
The timeline for the widespread availability of phage therapy depends on several factors:
- Regulatory Approval: As regulatory agencies establish clearer guidelines for phage therapy, the approval process for phage products will become more streamlined. The recent guidance from the MHRA is a positive step towards facilitating the development and approval of phage therapies.
- Clinical Trials: The outcomes of ongoing clinical trials will significantly impact the acceptance and availability of phage therapy. Successful trials demonstrating safety and efficacy could lead to quicker approvals and wider use in clinical settings.
- Infrastructure Development: The establishment of Good Manufacturing Practice (GMP)-compliant facilities for phage production and the creation of phage banks will be crucial for scaling up production. Investment in these infrastructures will help meet the demand for phage therapies.
- Public Awareness and Acceptance: Increased awareness and education about phage therapy among healthcare professionals and the public will be essential for its acceptance. As more success stories are shared and misconceptions are dispelled, acceptance may grow.
- Collaborations and Funding: Partnerships between public health organisations, research institutions, and private companies can accelerate the development and commercialisation of phage therapy. Increased funding for research and infrastructure will also play a vital role.
While it is challenging to predict an exact timeline, many experts believe that with continued advancements in research and regulatory support, phage therapy could become more widely available within the next few years. However, it may take longer for it to become a standard treatment option in clinical practice, particularly in regions where regulatory frameworks are still evolving.
Pros and Cons of Using Phages in Human Infections
Pros of Phage Therapy
- Targeted Action: Phages specifically target bacterial pathogens, allowing for effective treatment without harming beneficial bacteria in the microbiome. Research by Chan et al. (2013) indicates that phage therapy can selectively kill pathogenic bacteria while preserving the overall microbial community, minimising side effects associated with broad-spectrum antibiotics.
- Efficacy Against Antibiotic-Resistant Bacteria: Phage therapy has shown promise in treating infections caused by antibiotic-resistant bacteria. A study by Schooley et al. (2017) reported successful outcomes in a patient with a multidrug-resistant Acinetobacter baumannii infection treated with a customised phage cocktail, highlighting the potential of phages in addressing the growing issue of antibiotic resistance.
- Rapid Development and Adaptation: Phages can be rapidly isolated from the environment, allowing for quick development of therapeutic options in response to emerging bacterial infections. A review by Pires et al. (2016) explains that phages can be engineered or selected to target specific bacteria, providing a flexible approach to treatment.
- Potential for Personalised Treatment: Phage therapy allows for the creation of personalised phage cocktails tailored to match the specific bacterial strain infecting a patient. Research indicates that personalised phage preparations can enhance treatment efficacy and reduce the risk of resistance development (Dedrick et al., 2019).
- Minimal Collateral Damage: Since phages specifically target bacterial cells, they lead to less disruption of the host’s microbiome compared to traditional antibiotics. A study by Abedon (2019) supports the notion that phage therapy can help maintain a healthy balance of microbial communities while effectively treating infections.
Cons of Phage Therapy
- Phage Resistance: Bacteria can develop resistance to phages, which poses a challenge for long-term treatment efficacy. Abedon (2019) discusses the potential for rapid evolution of phage-resistant bacterial strains, necessitating the ongoing development of new phage preparations to combat this issue.
- Ecological Impact: The introduction of phages into the environment for therapeutic use may disrupt local ecosystems. Research by Pires et al. (2016) highlights concerns that phages could unintentionally affect non-target bacterial populations, potentially leading to shifts in microbial diversity and ecological imbalances.
- Limited Knowledge of Long-term Effects: The long-term effects of phage therapy on human health and the environment are not fully understood. Anomaly (2020) cautions that while phage therapy holds promise, the potential for unintended consequences, such as the emergence of new pathogens, requires further investigation.
- Regulatory Challenges: The regulatory landscape for phage therapy remains complex and inconsistent, which can slow down the approval process and lead to variability in treatment protocols. Schooley et al. (2017) emphasise the need for clear guidelines to ensure the safe and effective use of phage therapies in clinical settings.
- Potential Immune Response: The human immune system may recognise phages as foreign entities, leading to immune responses that could reduce the effectiveness of treatment. Studies indicate that repeated exposure to phages can result in the development of neutralising antibodies, which may limit their therapeutic application (Dedrick et al., 2019).
- Production and Quality Control Issues: Producing phages in sufficient quantities and ensuring consistent quality can be challenging. Lin et al. (2021) discuss the importance of adhering to stringent quality control measures to guarantee that phage preparations are safe and effective for clinical use.
Conclusion
Phage therapy represents a paradigm shift in the fight against antibiotic-resistant infections. With its proven efficacy, growing body of evidence, and supportive regulatory frameworks, phage therapy is poised for broader acceptance in mainstream medicine. As we confront the looming threat of AMR, embracing innovative solutions like phage therapy is not just an option; it is a necessity. Continued research, investment, and regulatory support will ensure that phage therapy becomes a cornerstone in the battle against drug-resistant infections, offering new hope to patients worldwide.
References
- Abedon, S. T. (2019). Bacteriophage Ecology. Current Topics in Microbiology and Immunology, 421, 1-25. DOI: 10.1007/82_2019_26.
- Anomaly, J. (2020). The Future of Phage: Ethical Challenges of Using Phage Therapy to Treat Bacterial Infections. Public Health Ethics, 13(1). DOI: 10.1093/phe/phaa003.
- Chan, B. K., Abedon, S. T., & Loc-Carrillo, C. (2013). Phage Cocktails and the Future of Phage Therapy. Future Microbiology, 8(6), 769–783. DOI: 10.2217/fmb.13.47.
- Cohen, E. J., et al. (2021). Advancements in Phage Therapy: Bridging the Gap to Clinical Practice. Journal of Bacteriology, 203(9), e00512-20. DOI: 10.1128/JB.00512-20.
- Dedrick, R. M., et al. (2019). Engineered Bacteriophages for Treatment of a Patient with a Disseminated Drug-Resistant Mycobacterium abscessus. Nature Medicine, 25(5), 730–733. DOI: 10.1038/s41591-019-0437-z.
- Gaus, G. F. (1998). Social Philosophy. London: Routledge.
- Hewitt, R., & Watson, P. (2013). Defining Biobank. Biopreservation and Biobanking, 11(5), 309–315. DOI: 10.1089/bio.2013.0042.
- Holt, K. E. (2017). The Rise of Antibiotic Resistance: A Global Challenge. Nature Reviews Drug Discovery, 16(7), 547-548. DOI: 10.1038/nrd.2017.87.
- Hyman, P., & Abedon, S. T. (2010). Bacteriophage Ecology. Bacteriophage, 1(2), 1-3. DOI: 10.4161/bact.1.2.14163.
- Kaye, J. (2010). Selected Legislation and Jurisprudence OECD Guidelines on Human Biobanks and Genetic Research Databases. European Journal of Health Law, 17(2), 187–204. DOI: 10.1163/157180910×12665776638821.
- Lin, R. C., et al. (2021). Phage Biobank: Present Challenges and Future Perspectives. Current Opinion in Biotechnology, 68, 221–230.
- Schooley, R. T., et al. (2017). Development and Use of Personalized Bacteriophage-Based Therapeutic Cocktails to Treat a Patient with a Disseminated Resistant Acinetobacter baumannii Infection. Antimicrobial Agents and Chemotherapy, 61(10). DOI: 10.1128/aac.00954-17.
- Wright, A., et al. (2018). The Role of Phage Therapy in the Fight Against Antibiotic Resistance. Nature Reviews Microbiology, 16(7), 415-424. DOI: 10.1038/s41579-018-0011-3.

